A leaked letter shows how OBGYNs disregard emotional health in childbirth. Here is how this traumatizes birthing people

As a clinical psychologist specializing in birth trauma, I’m all-too-familiar with the many ways the medical experience of childbirth – which 33-45% of birthing people report as being a traumatic experience – can lead to poor mental health outcomes. My clients say, and research confirms, that the most profound components of birth trauma are the experiences of being stripped of dignity in the birthing process, feeling uncared for, and feeling like the birthing person wasn’t treated as an individual.
But I’ve never seen written evidence that some doctors practice in a way that directly causes these adverse outcomes – until now. Late last week, a letter addressed to “expectant mothers” (though not all birthing people identify as women) from a group of obstetricians affiliated with Weill Cornell Medical College of New York Presbyterian Hospital in New York caused outrage among parents and providers alike after being circulated online. The reach of online birth justice communities meant that, moments after being shared, the post ricocheted far beyond its origins.
But I’ve never seen written evidence that some doctors practice in a way that directly causes these adverse outcomes – until now.
In the letter, reportedly included in new-patient information packets, the doctors discouraged patients from creating birth plans, which expectant parents use to outline the experience they hope to have during labor and delivery, from whether they prefer epidurals to what sort of music should play in the birthing room.
The doctors wrote that, while they would love for their patients to have the “perfect birth,” they feel that “the use of birth plans too frequently sets up unrealistic expectations and conditions for potential conflict. We are your care givers and would like to use our knowledge and experience to act in the best interest of you and your baby.”
Weill Cornell has since disavowed the letter, writing in an instagram post that it was “erroneously” included in recent information packets to patients (some recent patients expressed doubt about that in the post’s comments).
"We are your care givers and would like to use our knowledge and experience to act in the best interest of you and your baby."
But it doesn’t much matter whether the letter was given out in error or the hospital is backtracking for PR. The fact that it exists at all is concrete evidence of the widespread trauma birthing people experience regularly at the hands of medical professionals: perinatal mood and anxiety disorders are the most common complications of childbirth. And it shows what my clients have been telling me for years: that medicalized birth is in crisis, and urgently needs reform.
The United States has the worst childbirth-related mortality and severe maternal morbidity (i.e. “near misses”) rates of any other developed nation, with higher adverse outcome rates in birthing people of color. This is related to a confluence of factors, including systemic oppression and racism in medicine, and the U.S.’s profit-driven healthcare system. But it’s also due to the way physicians are still trained to prioritize medical interventions ahead of the people on whom they perform them (Lown, 2014).
Medicalized birth is in crisis, and urgently needs reform.
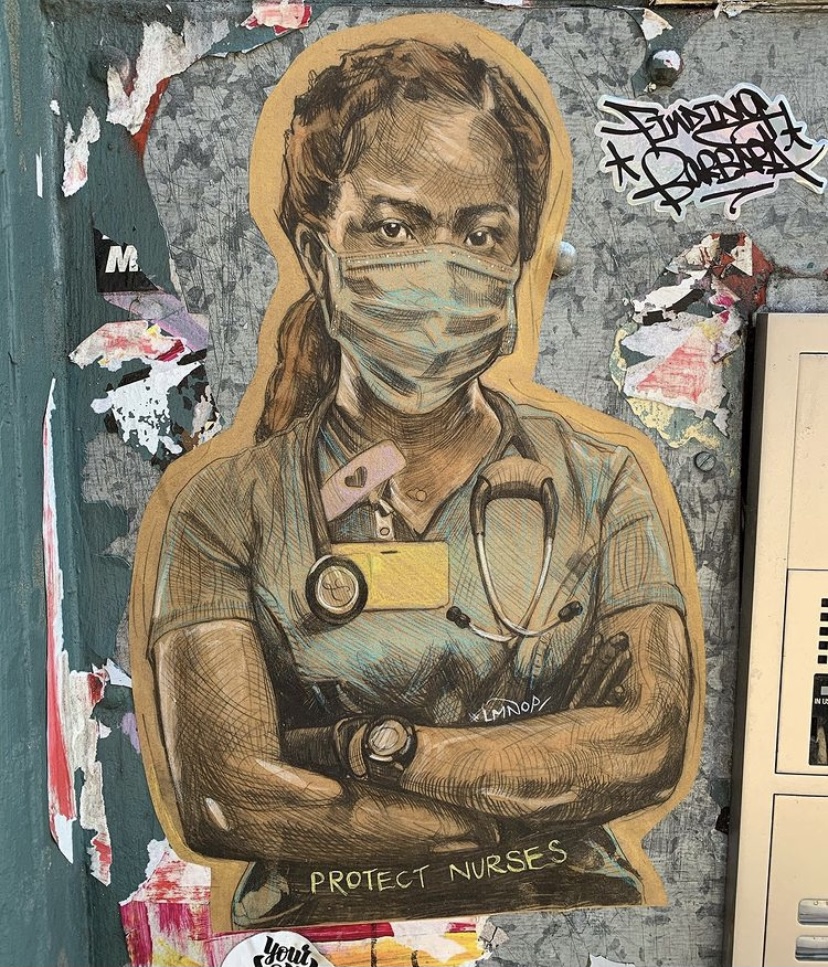
This includes when doctors diminish patient birth plans, which in my clinical experience is a tool for empowerment and education for the birthing person. To discount patient priorities around labor and delivery is to look at them as bodies rather than people, which leaves emotional health out of the care equation.
This is a recipe for birth trauma in and of itself, but the letter goes even further.
The doctors write, “Some of you may have specific questions about episiotomies, labor induction or augmentation, forceps or vacuum delivery, fetal monitoring or anesthesia in labor. We believe in giving our patients the best of care. In modern obstetrics, this may still include the aforementioned procedures.” This is a scary series of sentences meant to frighten birthing parents into compliance, further silencing any person-centered dialogue in the medical relationship.
In a country where the future of reproductive rights hinges on the opinions of a small group of conservative judges, the medical system must do better.
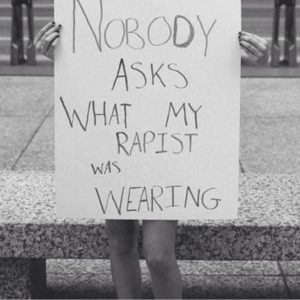
This is the opposite of what should be happening to start lowering the numbers of people who experience trauma symptoms after childbirth. Given that many birthing people are also survivors of sexual trauma or assault, we need to be focusing on improving trauma-informed obstetric care to this population. Nixing birthing plans does not accomplish this. Doctors need to take time to get to know their patients as human beings to protect their physical and emotional health during the birthing process.
In a country where the future of reproductive rights hinges on the opinions of a small group of conservative judges, the medical system must do better. Obstetrics must do better. People have a right to agency and choices in childbirth. Life-threatening emergencies happen where swift intervention is necessary, but there is no need to shut down communication prematurely.
About Us
At Center Psychology Group in New York, we specialize in providing compassionate and evidence-based therapy tailored to your unique needs. Whether you’re seeking EMDR therapy, Somatic Experiencing, or integrative trauma-informed psychotherapy, our experienced team is here to support you. Learn more about our services and how we can help you on the path to healing. Ready to take the next step in your healing journey? Book a free 15-minute phone consultation here.